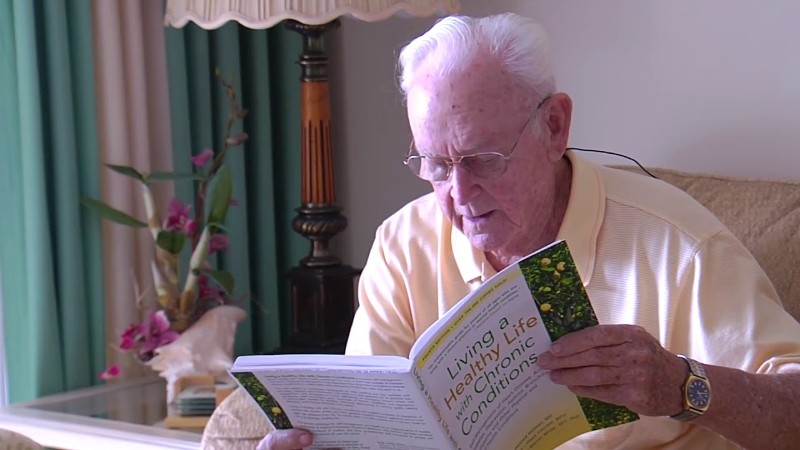
Polypharmacy, or the use of multiple medications, is common among older adults managing chronic health conditions. While necessary at times, it carries serious risks. About one-third of older adults in their 60s and 70s take five or more prescriptions, raising the chances of harmful drug interactions and overmedication. To reduce these risks, clinicians and caregivers should prioritize managing polypharmacy and regularly review medication regimens.
Key Takeaways
Polypharmacy among older adults poses significant risks due to harmful drug interactions and overmedication, necessitating careful management and regular review of medication regimens.
- Clinicians and caregivers should prioritize managing polypharmacy by regularly reviewing medication regimens and identifying opportunities for deprescribing or consolidating treatments.
- Older patients are particularly vulnerable to adverse effects due to their bodies processing drugs differently, making it essential to monitor non-prescription medications and supplements as well.
- A collaborative approach involving healthcare providers, caregivers, and pharmacists is crucial in managing polypharmacy among older adults, ensuring safe medication management and a better quality of life.
Understanding polypharmacy and its risks
Polypharmacy is commonly defined as taking five or more medications, with the risks becoming more pronounced as the number of drugs increases. Geriatric specialist Ariel Green, M.D., Ph.D., explains that while medications play a vital role in managing chronic illnesses such as hypertension, diabetes, and heart disease, excessive use or poor management of these medications can lead to significant health issues.
Older patients are particularly vulnerable to adverse effects because their bodies process drugs differently, often making them more susceptible to side effects such as confusion, dizziness, or falls.
Milta O. Little, DO, a geriatrician, highlights the challenges of managing multiple medications in older adults, noting that standard disease management guidelines typically focus on single conditions rather than the complex scenarios where multiple medications are prescribed.
Little notes that patients frequently take ten or more medications, which can result in various issues such as cognitive decline, falls, and drug interactions. Addressing polypharmacy necessitates careful coordination among healthcare providers and may involve deprescribing, a systematic process for reducing unnecessary medications.
Common symptoms of polypharmacy
Polypharmacy in older adults can result in a range of symptoms, including reduced alertness, confusion, weakness, dizziness, and loss of balance, which may lead to falls. Gastrointestinal issues such as diarrhea or constipation are also common, along with skin rashes, depression, and anxiety.
These symptoms are often mistaken for typical signs of aging, but they may be linked to side effects from medications. Both Dr. Green and Dr. Little emphasize that when these symptoms arise, healthcare providers should first assess the patient’s medication regimen to identify potential causes related to polypharmacy.
Strategies for managing polypharmacy
Obtain a comprehensive medication list: It’s crucial to secure a complete list of all medications, including prescriptions, over-the-counter drugs, and supplements. Dr. Little highlights the importance of understanding how patients organize their medications to ensure safety and compliance, especially when multiple doctors are involved. Checking for duplication or unnecessary medications is essential.
Reorganize Medications in Electronic Health Records (EHRs): Medications in EHRs are typically listed alphabetically, but Dr. Little recommends organizing them by the conditions they treat, such as blood pressure or pain management. This approach makes it easier to identify opportunities for deprescribing or consolidating treatments and helps spot potential drug interactions quickly.
Identify and avoid drug-drug and drug-disease interactions: Managing polypharmacy requires vigilance regarding drug-drug interactions and ensuring that medications do not exacerbate other health issues. For instance, hypertension medications can cause dizziness, increasing fall risk. Regularly reassessing each medication’s appropriateness in light of the patient’s overall health can help mitigate these risks.
Regular medication reviews and deprescribing: Medication reviews should be routine, especially after significant health changes like hospitalizations or falls. Both Dr. Little and Dr. Green emphasize the importance of careful deprescribing to avoid withdrawal effects or worsening conditions.
Monitor non-prescription medications and supplements: Patients may take over-the-counter drugs or supplements without realizing their risks. Dr. Green notes that supplements like ginkgo biloba can interfere with blood thinners, raising bleeding risks. Healthcare providers must inquire about all substances a patient is taking, including non-prescription ones.
Caregivers and pharmacists as key partners
Caregivers and pharmacists play an essential role in monitoring and managing polypharmacy. Caregivers can help patients stick to medication schedules and ensure proper dosing, while pharmacists can review prescriptions for potential interactions and suggest adjustments.
This collaborative approach is particularly important for older adults managing multiple chronic conditions. “Medications must be tailored to the individual’s health priorities,” says Green, noting that factors such as mobility and cognitive function should guide medication decisions.
Managing polypharmacy in older adults involves regular medication reviews, monitoring for drug interactions, and strategic deprescribing. Collaboration with caregivers, pharmacists, and healthcare providers helps ensure safe medication management and a better quality of life.